Case Study: Rapid Rehabilitation After Sports Injuries
Sports injuries are an inevitable part of athletic life, impacting amateur and professional athletes.The path to recovery can be long and arduous, often fraught with challenges that test an athlete's physical and mental endurance. However, with the right approach to rehabilitation, the journey back to peak performance can be significantly accelerated.This case study delves into effective strategies for rapid rehabilitation after sports injuries, emphasizing practical methods and tools that have proven successful in real-world scenarios.
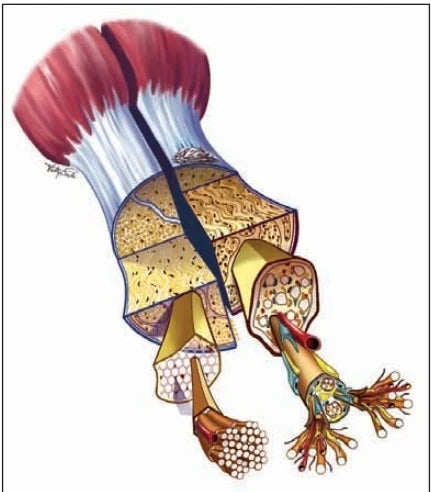
Understanding Sports Injuries
Sports injuries range from minor sprains and strains to severe fractures and dislocations. Common types include:
- Muscle Strains and Sprains: Overstretching or tearing of muscles and ligaments.
- Fractures: Breaks in the bone often caused by high-impact activities.
- Dislocations: Bones are forced out of their normal position.
- Tendonitis: Inflammation of the tendons, usually due to overuse.
- Concussions: Brain injuries resulting from blows to the head.
Each type of injury requires a tailored rehabilitation approach, considering the specific demands of the sport and the individual's health condition.
The Rehabilitation Process
Effective rehabilitation encompasses several phases, each crucial for a full and fast recovery. These phases include:
- Acute Phase: Focuses on pain management and minimizing swelling.
- Subacute Phase: Aims to restore joint range of motion and reduce muscle atrophy.
- Rehabilitation Phase: Involves strengthening exercises and functional training.
- Return-to-Play Phase: Prepares the athlete for the physical demands of their sport.
Let's explore these phases in detail through a case study of a fictional athlete, John, who experienced a severe ankle sprain while playing soccer.
CaseStudy: John’s Rapid Rehabilitation
Injury Description
John, a 25-year-old semi-professional soccer player, suffered a severe ankle sprain during a match. Immediate swelling and bruising indicated significant ligament damage, requiring a comprehensive rehabilitation plan to ensure a full and fast recovery.
Acute Phase
Objectives
- Reduce pain and inflammation
- Protect the injured area
Methods
- Rest and Immobilization: John was advised to rest his ankle and avoid weight-bearing activities. A brace was used to immobilize the joint.
- Ice Therapy: Applying ice packs for 20 minutes every two hours helped manage swelling and pain.
- Elevation and Compression: Keeping the ankle elevated above heart level and using a compression bandage further reduced swelling.
Outcome
After one week, John experienced a significant reduction in pain and swelling, allowing for the transition to the subacute phase.
Subacute Phase
Objectives
- Restore joint mobility
- Prevent muscle atrophy
Methods
- Gentle Range of Motion Exercises: John began performing ankle circles and alphabet exercises to maintain joint flexibility.
- Therapeutic Ultrasound: This helped reduce inflammation and promote tissue healing.
- Hydrotherapy: Gentle exercises in a pool minimize stress on the injured ankle while encouraging movement.
Outcome
Within three weeks, John regained a significant degree of ankle mobility and reduced muscle stiffness, setting the stage for more intensive rehabilitation exercises.
Rehabilitation Phase
Objectives
- Strengthen muscles
- Improve balance and proprioception
Methods
- Resistance Training: John incorporated resistance bands to strengthen the muscles around the ankle.
- Balance Exercises: Activities like standing on one leg and using a balance board improved his proprioception.
- Cardio Workouts: Low-impact activities such as cycling and swimming maintained his overall fitness without straining the ankle.
Outcome
After six weeks, John exhibited marked improvement in muscle strength and balance, feeling more confident in his ankle's stability.
Return-to-Play Phase
Objectives
- Prepare for sport-specific demands
- Ensure mental readiness
Methods
- Sport-Specific Drills: John began light jogging, dribbling drills, and agility exercises tailored to soccer.
- Plyometric Training: Jumping and bounding exercises enhanced his explosive power and reaction time.
- Psychological Support: Regular sessions with a sports psychologist helped John manage anxiety and build confidence in his fast recovery.
Outcome
By the end of three months, John returned to full training with his team, demonstrating no significant loss in performance or recurring pain.
Tools And Products For Rapid Rehabilitation
Throughout John's rehabilitation journey, several tools and products were vital to his fast recovery. These include:
- Compression Bandages and Braces: Essential for stabilizing the injured area during the acute phase.
- Ice Packs and Heat Pads: Effective for managing pain and inflammation.
- Resistance Bands: Crucial for progressive strength training exercises.
- Balance Boards: Helped improve proprioception and prevent future injuries.
- Therapeutic Devices: Ultrasound and hydrotherapy tools facilitated faster tissue healing and mobility restoration.
Best Practices For Rapid Rehabilitation
Based on John's experience, several best practices emerge for rapid rehabilitation:
- Early Intervention: Prompt and appropriate treatment during the acute phase sets the foundation for a fast recovery.
- Individualized Plans: Tailoring the rehabilitation program to the specific injury and the athlete's needs ensures more effective outcomes.
- Multidisciplinary Approach: Physical therapy, strength training, psychological support, and sport-specific drills combine to address all aspects of recovery.
- Patient Education: Educating athletes about injury prevention and proper techniques reduces the risk of future injuries.
Frequently Asked Questions (FAQs)
1. What is the difference between acute and chronic sports injuries?
Acute sports injuries occur suddenly during activity, often due to trauma or impact, such as sprains, fractures, or dislocations. Chronic sports injuries, on the other hand, develop over time due to repetitive stress on tissues, such as tendonitis or stress fractures.
2. How soon should I start rehabilitation after a sports injury?
Rehabilitation should begin immediately after the injury, ideally within 24-48 hours. Early intervention helps minimize swelling and pain, leading to a more effective and fast recovery.
3. What role does nutrition play in sports injury rehabilitation?
Proper nutrition is crucial for fast recovery. A protein-rich diet, vitamins, and minerals supports tissue repair and reduces inflammation. Staying hydrated and consuming anti-inflammatory foods like leafy greens, berries, and omega-3 fatty acids can enhance healing.
4. Can I continue training other body parts while recovering from a sports injury?
Yes, you can continue training non-injured parts of your body. This approach, known as "cross-training," helps maintain overall fitness and strength without stressing the injured area.
5. How important is sleep in the rehabilitation process?
Sleep is vital for recovery as it promotes muscle repair and reduces inflammation. Aim for 7-9 hours of sleep per night to support your body's healing processes.
6. What are some signs that I might be pushing too hard during rehabilitation?
Signs of overexertion include increased pain, swelling, and stiffness in the injured area, fatigue, and decreased performance. If you experience these symptoms, you must reduce the intensity of your rehabilitation exercises and consult your healthcare provider.
7. Are there any risks associated with rapid rehabilitation?
While rapid rehabilitation aims to speed up recovery, pushing too hard too soon can risk re-injury or prolonged healing. It is important to follow a structured and progressive rehabilitation plan tailored to your specific injury and needs.
8. How can mental health impact the rehabilitation process?
Mental health plays a significant role in rehabilitation. Anxiety, stress, and depression can negatively impact recovery. Engaging in mental health support, such as counseling or mindfulness practices, can enhance your overall rehabilitation experience.
9. Is it necessary to see a specialist for every sports injury?
While minor injuries might be managed with basic first aid and self-care, more serious or persistent injuries should be evaluated by a healthcare professional, such as a sports physician or physical therapist, to ensure proper treatment and prevent complications.
10. What types of exercises are typically included in a rehabilitation program?
Rehabilitation programs usually include a mix of:
- Flexibility exercises: To maintain or improve joint range of motion.
- Strengthening exercises: To build muscle around the injured area.
- Balance and proprioception exercises: To enhance coordination and prevent future injuries.
- Cardio workouts: Low-impact activities to maintain overall fitness.
11. How can I prevent sports injuries in the future?
Preventing sports injuries involves:
- Proper warm-up and cool-down routines: Preparing muscles and joints for activity.
- Strength and conditioning programs: Building overall fitness and resilience.
- Using proper equipment and techniques: Ensuring correct form and support.
- Listening to your body: Resting and recovering adequately to avoid overuse injuries.
12. What is the role of physical therapy in sports injury rehabilitation?
Physical therapy is integral to rehabilitation. It focuses on restoring function, improving mobility, and preventing further injury. Therapists use a combination of manual therapy, exercise prescriptions, and educational guidance tailored to each patient's specific needs.
13. Can alternative therapies aid in sports injury recovery?
Alternative therapies such as acupuncture, chiropractic care, and massage therapy can complement traditional rehabilitation methods. They may help reduce pain, improve circulation, and promote relaxation, contributing to overall recovery.
14. How do I know when I’m ready to return to sports?
You’re ready to return to sports when you have:
- Full range of motion: Comparable to the non-injured side.
- Strength and endurance: Equal to pre-injury levels.
- No pain or swelling: During or after activities.
- Confidence: In the injured area’s stability and function. Always consult with your healthcare provider to confirm your readiness.
15. What should I do if I experience a setback during rehabilitation?
If you experience a setback, such as increased pain or a new injury, stop the activity immediately and consult your healthcare provider. Adjustments to your rehabilitation plan may be necessary to ensure safe and effective recovery.
Enhancing Recovery With Heal Faster Canada
John's journey highlights the importance of a structured and comprehensive rehabilitation program. By following a systematic approach and utilizing effective tools, athletes can rapidly recover and confidently return to sports.
For those seeking to enhance their rehabilitation process, Heal Faster offers a wide range of products to support every recovery phase. Heal Faster provides the tools for a swift and successful return to peak performance, from compression bandages and resistance bands to advanced therapeutic devices.
Explore our offerings at Heal Faster and take the first step towards a more effective and fast recovery today.